Health care is entering a new era, one that moves closer to where people live.
By 2026, the traditional model of care, centered around hospitals and clinics, is giving way to a more decentralized, patient-centric approach. This shift is driven by three converging forces: rising costs, evolving patient expectations and technological advancements that make care delivery more flexible and responsive.
The rise of hospital-at-home programs exemplifies this transformation. These models enable patients to receive acute-level care in the comfort of their own homes, supported by remote monitoring technologies and virtual clinical teams. Forecasts suggest that home health spending is expected to surge, driven by increasing demand for in-home and community-based care.
Why hospital-at-home is gaining momentum
For patients, the benefits are clear: they can recover in familiar surroundings, avoid the stress and risks associated with hospital stays (such as hospital-acquired infections) and experience greater autonomy in their care journey. Studies have shown that patients treated at home often experience faster recovery times, fewer readmissions and higher satisfaction rates.
For providers, the model offers a way to reduce costs, alleviate capacity constraints and improve operational efficiency. By shifting appropriate cases out of the hospital, health systems can free up beds for more critical patients and reduce overhead expenses. Moreover, the data generated through remote monitoring can help clinicians make more informed decisions, leading to better outcomes and more personalized care.
Still, challenges remain. Reimbursement models are still evolving slowly. Staffing remains a concern, particularly among clinicians trained for remote patient management. And the technical challenges of integrating data from multiple devices into electronic health records (EHRs) continue to limit interoperability.
Technology is making it possible
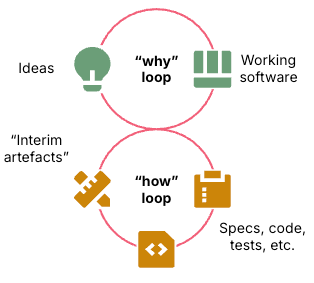
At the heart of the hospital-at-home movement is data. IoT devices, ranging from wearable sensors to smart home systems, generate substantial streams of information on patient vitals, activity levels and medication adherence.
Event stream processing and AI make this data actionable. Streaming analytics tools enable real-time monitoring, enabling the detection of anomalies or early warning signs as they occur. AI models interpret these data patterns to identify risk, predict deterioration and recommend interventions before a crisis arises.
For example, in patients with congestive heart failure, IoT-enabled scales and blood pressure monitors can track weight gain and blood pressure fluctuations, early indicators of fluid retention. AI models can analyze these trends and alert clinicians to intervene before the patient requires hospitalization. This proactive approach not only improves outcomes but also reduces costs and enhances the patient experience.
Early success stories and demonstration projects
While the hospital-at-home model has been proven to improve outcomes, the digital layer that powers it is still in its early stages of development. Early adopters are beginning to validate how.
Mount Sinai’s hospital-at-home has shown promising results in reducing readmissions and improving patient satisfaction. Similarly, Mayo Clinic and Kaiser Permanente have invested in virtual care platforms that support home-based acute care.
These early adopters are generating additional data-driven evidence that will be critical in shaping future funding and policy decisions. As more organizations share their outcomes, payers and regulators will gain confidence in the model’s efficacy and scalability. This, in turn, will accelerate adoption and spur innovation across the ecosystem.
Looking ahead: A data-driven future for care
Hospital-at-Home is more than a trend – it’s a structural shift in how health care is delivered. To realize its promise, alignment across the ecosystem is essential:
- Payers must create reimbursement models that reward value-based, home-delivered care.
- Providers must invest in training, infrastructure, and workflows that support hybrid clinical teams.
- Technology innovators must prioritize secure, interoperable and user-friendly solutions.
Equity must also remain central. Not every patient has access to high-speed internet, smart devices, or at-home support systems. Addressing these disparities will be critical to ensuring digital transformation benefits all.
The future of health care is decentralized, data-driven and deeply human. By combining the intelligence of AI with the reach of IoT, we can extend care beyond hospital walls – delivering proactive, personalized and efficient health care wherever patients call home.