In healthcare software, quality is inseparable from compliance. A feature working as designed is not enough. Every workflow, integration, and data exchange must protect Protected Health Information and withstand regulatory scrutiny.
Healthcare organizations operate under strict requirements defined by the Health Insurance Portability and Accountability Act. HIPAA compliance in healthcare software is not an optional enhancement. It is a foundational expectation from regulators, enterprise buyers, providers, and patients.
From a QA leadership perspective, one recurring pattern appears across healthcare product teams. HIPAA is often treated as a milestone activity. Teams validate compliance shortly before go live or during a formal audit cycle. This late validation introduces stress, rework, and risk.
HIPAA readiness must be built into the QA lifecycle from day one. It must be continuous, measurable, and supported by evidence.
This guide explores how AI powered HIPAA compliance readiness testing transforms healthcare software quality assurance. It outlines practical QA artifacts, risk governance models, readiness scorecards, and a modern approach that moves beyond static checklists toward continuous compliance intelligence.
What HIPAA Compliance Means in Healthcare Software
HIPAA defines national standards for protecting electronic Protected Health Information.
For healthcare software companies, this translates into concrete responsibilities:
- Control who can access patient data
- Protect how PHI is stored and transmitted
- Log and audit every access event
- Prevent unauthorized disclosure
- Maintain safeguards against misuse
HIPAA compliance in healthcare software extends beyond infrastructure security. Application level behavior must align with regulatory safeguards. This includes user interface visibility rules, API responses, integration workflows, error handling, and audit traceability.
For leadership teams, HIPAA compliance represents:
- Regulatory protection against civil penalties
- Defense against breach related litigation
- Trust assurance for patients and partners
- Market access into enterprise healthcare ecosystems
For QA teams, HIPAA compliance testing means validating that safeguards are implemented consistently and provably. Evidence matters. Traceability matters. Reproducibility matters.
The Business Impact of HIPAA and PHI Non Compliance
HIPAA non compliance is not abstract risk. It produces measurable financial, operational, and reputational damage.
Financial Penalties and Regulatory Action
The U.S. Department of Health and Human Services Office for Civil Rights enforces HIPAA regulations. Civil monetary penalties can range from thousands to millions of dollars depending on violation severity and duration. Repeated failures often lead to corrective action plans and ongoing oversight.
Breach Response and Remediation Costs
Beyond regulatory fines, breach remediation costs include:
- Incident investigations
- Forensic analysis
- Legal consultation
- Public notification requirements
- System redesign and remediation
- Credit monitoring for affected patients
Healthcare data breaches consistently rank among the most expensive across industries due to the long term sensitivity of PHI.
Operational Disruption
HIPAA incidents frequently trigger:
- Emergency audits
- Engineering resource diversion
- Development freezes
- Release delays
- Security reassessment across modules
Product roadmaps stall while teams shift to compliance firefighting.
Loss of Trust
Healthcare is built on trust. A HIPAA violation can erode patient confidence, strain relationships with providers and payers, and complicate enterprise contracts.
Delayed Certifications and Market Access
Healthcare startup software vendors often face extensive security reviews during enterprise sales cycles. Without clear HIPAA compliance readiness artifacts, onboarding slows. Deals stall. Certifications delay.
From a business perspective, preventive HIPAA readiness testing costs significantly less than post incident remediation.
Organizations that embed HIPAA compliance testing into QA processes gain:
- Predictable audits
- Faster certifications
- Reduced breach risk
- Stronger brand credibility
Why HIPAA Readiness Is a QA Challenge
A common misconception is that HIPAA compliance belongs solely to security or legal teams. In practice, many HIPAA controls become meaningful only when validated through application behavior.
QA teams must validate:
- Role based access control across dynamic workflows
- Data masking across UI components and exports
- Audit log completeness
- Session management enforcement
- Error response safety
- Integration level PHI handling
Compliance requirements are often context driven. Risks emerge through edge cases, integration flows, and failure conditions rather than standard happy path testing. HIPAA gaps rarely result from missing features. They emerge from untested paths, inconsistent enforcement, and missing evidence. QA functions as the bridge between compliance intent and operational reality.
Defining HIPAA Compliance Readiness
Being HIPAA ready does not mean claiming compliance certification. It means demonstrating readiness through evidence.
HIPAA compliance readiness includes:
- Clear mapping between regulatory controls and product features
- Validated test coverage for PHI related functionality
- Documented risk management decisions
- Audit ready evidence repositories
- Continuous monitoring of compliance posture
HIPAA readiness is not a quarterly event. It is a living state supported by ongoing QA validation.
Core QA Validation Areas for HIPAA Compliance
PHI Data Flow and Transfer Validation
QA must validate how PHI moves across:
This includes encryption in transit and at rest, log sanitization, secure error handling, and prevention of data leakage across system boundaries.
Role Based Access Control Testing
RBAC testing ensures users access only appropriate PHI based on defined roles.
QA validates:
- Authorized access scenarios
- Unauthorized access attempts
- Role transitions
- Privilege escalation attempts
- Edge cases across shared accounts
Authentication and Session Management Testing
QA validates secure login mechanisms, session timeout enforcement, token expiration, and re authentication triggers for sensitive workflows.
Audit Logging and Traceability Testing
HIPAA requires that PHI access is logged with sufficient detail.
QA verifies:
- Who accessed data
- What data was accessed
- When access occurred
- From which context
Logs must be retrievable and consistent with audit expectations.
Data Masking and Visibility Controls
Sensitive information must be masked or restricted in:
- Reports
- Exports
- APIs
- Screenshots
- Administrative dashboards
QA validates that masking rules persist across product changes.
Error Handling and Exception Scenarios
System failures often expose PHI inadvertently. QA must test:
- Validation failures
- API errors
- Timeout responses
- Database errors
PHI must never appear in error messages or stack traces.
QA Artifacts That Enable HIPAA Readiness
HIPAA Mapped Test Scenarios
These scenarios explicitly map product behaviors to regulatory controls. They cover:
- Access validation
- Data exposure
- Logging requirements
- Encryption checks
- Edge case handling
HIPAA Readiness Checklist
A structured checklist tracks safeguard coverage across releases. It ensures no control is overlooked during iterative development.
HIPAA Readiness Scorecard
The readiness scorecard provides leadership with a measurable view of compliance posture. It reflects:
- Control coverage
- Test execution results
- Open compliance risks
- Evidence completeness
QA Owned Risk Register
The risk register documents:
- Identified compliance gaps
- Severity and likelihood
- Mitigation strategies
- Acceptance decisions
This ensures transparency and executive visibility.
Building a HIPAA Compliance Readiness Testing Application
To operationalize readiness, healthcare teams benefit from a centralized HIPAA compliance readiness platform.
Such an application consolidates:
- Mapped HIPAA controls
- Test case execution data
- Risk tracking dashboards
- Evidence repositories
- Compliance scorecards
This replaces scattered spreadsheets and manual follow ups with structured governance. The application becomes a single source of truth for compliance posture.
Leveraging AI for Continuous HIPAA Readiness Assessment
Traditional compliance testing relies on static checklists. Modern healthcare software environments evolve rapidly. Static models fail to keep pace.
AI powered HIPAA compliance readiness testing introduces intelligence into the QA lifecycle.
An AI assisted readiness scorecard analyzes structured inputs such as:
- Pass fail status of compliance tests
- Severity weighting of failed controls
- Evidence completeness
- Open risk remediation progress
- Historical trend data
Instead of manual aggregation, AI models interpret patterns across these signals and generate a dynamic readiness score.
This score reflects actual implementation health rather than superficial test completion metrics.
Benefits of AI driven compliance monitoring include:
- Continuous posture evaluation
- Early detection of emerging compliance gaps
- Objective readiness scoring
- Reduced manual reporting overhead
- Improved executive decision support
AI functions as a decision support layer. QA retains ownership of validation. Leadership gains real time visibility into risk.
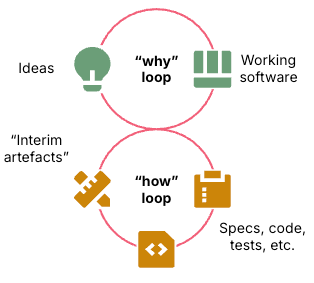
Embedding HIPAA Compliance in the Secure SDLC
Continuous HIPAA compliance requires integration into the Secure Software Development Lifecycle.
Requirements Phase
Compliance controls are translated into testable acceptance criteria.
Design Phase
Architectural decisions incorporate encryption, RBAC, and logging safeguards.
Development Phase
Developers follow secure coding standards aligned with HIPAA expectations.
Testing Phase
QA validates safeguards through mapped scenarios and automated checks.
Release Phase
Readiness scorecards inform go no go decisions.
Post Release Monitoring
AI powered analytics monitor compliance posture over time.
This lifecycle approach reduces audit surprises and minimizes rework near go live.
Why Continuous HIPAA Readiness Matters to Healthcare Product Teams
When HIPAA compliance testing is QA led and continuous:
- Audit surprises reduce significantly
- Rework close to launch declines
- Leadership gains confidence in release decisions
- PHI protection becomes measurable
Compliance shifts from reactive to proactive.
How ISHIR Helps Healthcare Organizations Achieve HIPAA Readiness
ISHIR supports healthcare organizations with AI powered HIPAA compliance readiness testing integrated into digital product engineering.
Our healthcare QA and security teams help clients:
- Map HIPAA controls to application features
- Design compliance focused test frameworks
- Implement AI driven readiness scorecards
- Establish QA owned risk registers
- Build centralized compliance dashboards
- Embed compliance validation into agile delivery cycles
We serve clients across Texas including Dallas Fort Worth, Austin, Houston, and San Antonio. Our North American footprint extends to Canada including Toronto and Vancouver. We support organizations in Singapore and the UAE including Abu Dhabi and Dubai.
Our delivery teams operate across Asia including India, Nepal, Pakistan, and Vietnam, across LATAM including Argentina, Brazil, Chile, Colombia, Costa Rica, Mexico, and Peru, and across Eastern Europe including Estonia, Kosovo, Latvia, Lithuania, Montenegro, Romania, and Ukraine. We also extend services across the Gulf Cooperation Council including Bahrain, Kuwait, Oman, Qatar, and Saudi Arabia.
Through structured QA governance and AI driven compliance intelligence, ISHIR helps healthcare product teams move from periodic HIPAA checks to continuous compliance readiness.
Manual checklists and periodic reviews can’t keep up with evolving PHI risks in modern healthcare applications.
Implement AI driven compliance monitoring with readiness scorecards, mapped QA artifacts, and real-time risk visibility.
Frequently Asked Questions About AI Powered HIPAA Compliance Readiness Testing
Q. What is AI powered HIPAA compliance readiness testing in healthcare software?
AI powered HIPAA compliance readiness testing combines traditional QA validation with intelligent scorecards that analyze test results, risk severity, and evidence completeness. It provides continuous visibility into compliance posture rather than periodic audit preparation. This approach improves healthcare software security testing accuracy.
Q. How does HIPAA compliance testing differ from functional testing?
Functional testing verifies feature behavior. HIPAA compliance testing validates whether PHI safeguards hold under real world conditions, including edge cases and failure scenarios. It focuses on regulatory control enforcement and audit traceability.
Q. Why should QA own HIPAA readiness artifacts?
QA teams validate real application behavior. They maintain traceable evidence, mapped test cases, and risk documentation. This makes QA central to demonstrating HIPAA readiness during audits.
Q. What is a HIPAA readiness scorecard?
A HIPAA readiness scorecard is a structured evaluation tool that aggregates compliance test results, open risks, and evidence completeness into a measurable readiness metric. AI driven scorecards enhance objectivity and consistency.
Q. How does AI improve healthcare compliance monitoring?
AI interprets patterns across compliance signals, detects emerging risk trends, and continuously updates readiness scores. It reduces manual reporting and strengthens executive visibility.
Q. What QA artifacts should be audit ready at all times?
Healthcare teams should maintain mapped compliance test scenarios, execution logs, audit log verification records, risk registers, readiness checklists, and scorecards.
Q. When should HIPAA compliance testing begin?
HIPAA compliance testing should begin during requirements and design phases. Early integration reduces remediation cost and prevents audit delays.
Q. Can HIPAA readiness scale with agile development?
Yes. Reusable test frameworks, standardized checklists, and AI powered monitoring allow HIPAA compliance to scale alongside rapid feature iteration.
Q. How does RBAC testing support HIPAA compliance?
Role based access control testing ensures users access only appropriate PHI. It prevents overexposure and reduces breach risk.
Q. What risks arise from late stage compliance validation?
Late validation increases rework, delays releases, heightens audit risk, and amplifies remediation costs.
Q. How does a QA owned risk register improve compliance governance?
A QA owned risk register documents identified compliance gaps, severity ratings, and mitigation plans. It ensures executive visibility and informed risk decisions.
Q. What role does audit logging testing play in HIPAA readiness?
Audit logging testing verifies traceability of PHI access events. It ensures logs contain required metadata and remain retrievable during regulatory review.
Q. How do healthcare software vendors demonstrate HIPAA readiness to enterprise buyers?
They present structured evidence including control mapped test cases, readiness scorecards, and documented risk management practices.
Q. Is AI replacing QA in HIPAA compliance testing?
No. AI enhances decision support and posture monitoring. QA remains responsible for validation, evidence, and governance.
Q. How does continuous HIPAA readiness reduce business risk?
Continuous readiness reduces breach likelihood, accelerates audits, shortens enterprise sales cycles, and strengthens patient trust.
Enabling Smooth HIPAA Certification Through Strong QA
HIPAA certification delays rarely result from lack of effort. They stem from missing evidence, late discovery of risks, and inconsistent safeguard validation.
A robust QA framework embedded with AI powered compliance intelligence transforms readiness into a continuous discipline.
By maintaining mapped controls, structured artifacts, readiness scorecards, and transparent risk registers, healthcare organizations approach HIPAA audits with confidence rather than urgency.
In modern healthcare software development, protecting patient data is inseparable from delivering product quality. AI powered HIPAA compliance readiness testing ensures both objectives advance together.